Distal Femur Fracture
What is a Distal Femur Fracture?
A distal femur fracture is a break of the thigh bone just above the knee. It can result in cracks that extend into the knee joint itself. They can also happen around total joint replacements. These fractures usually result from high energy injuries such as car accidents in younger patients and most often from falls in the elderly patient. The distal femur can be broken into many pieces or just crack slightly depending on the quality of bone and the type of injury.
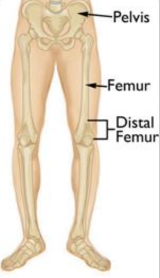
Illustration of distal femur bone. Reproduced with permission from OrthoInfo. © American Academy of Orthopaedic
Surgeons. https://orthoinfo.org/
What does the Distal Femur do?
The distal femur is an important part of the knee joint because it forms the entire top half of the joint and the grove that the knee cap travels in. The strong ligaments and tendons of the knee attach to the distal femur and allow for knee strength and stability. The distal femur is also covered with a layer of cartilage that allows the knee to glide smoothly. If this is disrupted, arthritis can occur.
Diagnosis and Examination
Physical examination is critical in the evaluation of these injuries. Important nerves and blood vessels run next to this bone and can be injured when it breaks. Diagnosis of an injury to some blood vessels requires urgent surgery. The doctor will look for any open wounds over the injury as these usually require surgery. Often, the bone tries to poke out of the skin or “tent.” If this is not corrected, the skin can die or the bone can eventually cut the skin.
X-rays are used to evaluate the location and severity of the broken bone. This helps doctors and patients make an informed decision on treatment. Often 2 or more x-rays are taken to show the injury pattern. A CT(Computed Tomography) scan is often ordered to help plan treatment and surgery. Sometimes an MRI is ordered for small fractures or to help diagnose stress fractures that do not show up on plain x-rays.

Preoperative CT scan of distal femur fracture.

Preoperative x-ray of distal femur fracture.
Non-Surgical Treatment for Distal Femur Fractures
Very few distal femur fracture patterns and types do not need surgery for the bone to heal. This is because the strength of muscles that pull on the bones trying to pull them apart. Small breaks or those with good overall alignment often can be treated without an operation. Nonsurgical treatment is also recommended for adults with poor overall health, fragile or chronically infected skin and less active patients. Knee immobilizers, hinged knee braces and casts are all used to treat these injuries depending on the fracture type and patient characteristics.
If non-operative care is chosen, regular follow-up care for a physical exam and x-rays is important to ensure that the fracture stays in good position and heals appropriately. Cutting down or quitting smoking and tight blood sugar control if you are a diabetic is important for the healing process. One fall or continued lack of compliance with casting, bracing or early walking against medical advice can cause bones to move and result in the need for surgery.
Depending on health and injury pattern this bone can take 3-4 months to heal without surgery. Physical therapy for knee range of motion is started around 6 weeks once bone has healed enough to prevent displacement with motion.
Surgical Treatment for Distal Femur Fractures
Surgeons may recommend an operation to femur fracture if the pieces are displaced, if the bone sticks out of the skin, if skin is at risk for dying or if the bone is unstable due to the fracture type. The distal femur can be fixed with metal plates and screws or intramedullary nails. If the break involves the joint or is around a total knee replacement it is usually fixed with metal plates and screws placed through incisions on the side of the leg. Surgery usually takes 1 to 2 hours. Most patients are admitted overnight.
In cases where there is severe injury to the muscles, nerves or arteries or there is significant contamination with dirt, rocks or grass from the injury, some patient require external fixation prior to definitive surgical treatment. This is an operation where metal pins are placed into the bone through small cuts and connected to bars to give some stability to the bone. After secondary operations to clean the wound or recovery of skin injuries, the external fixator can be removed and plates and screws can be placed.
Ideally, surgeons like to perform this surgery acutely or at most within 1-2 weeks of injury. Thus, patients have time to seek a second opinion regarding treatment if more information or additional surgeon input is desired.
It is important to choose your surgeon wisely. Extensive surgical experience can be helpful in achieving a good result and avoiding complications. Collectively, ROC surgeons have performed more distal femur operations than any practice in Northern Nevada and take pride in outstanding surgical results.
After surgery, patients are often placed in a knee immobilizer or hinged brace. They cannot bear weight immediately. Patients will need to use a walker or crutches for the first six weeks. Gentle motion of the knee is begun early to prevent stiffness. Gradually this motion is increased and physical therapy is begun around six weeks after surgery if the patient has residual knee or ankle stiffness. Your doctor may decide to put you on a blood thinner after surgery for 2-6 weeks depending on your risk factors.

Distal Femur Post-Op X-Ray
Surgical Complications
Complications can occur with any surgery, no matter how small. There is always a risk of infection. The risk is much bigger for larger and more contaminated traumatic wounds. A dose of antibiotics given prior to surgery helps to make this risk as small as possible. There is always a risk of injury to blood vessels or nerves. This is reduced by having an experienced surgeon involved in your care. As stated above, compartment syndrome can occur from the injury and evolve during surgery. This requires additional surgery to release the pressure on the muscles. Noncompliance with weight bearing restrictions, too much motion or falls can result in the metal ripping out of the bone or the fracture separating. It is always possible that the bone may not heal and additional surgery will be required. This is usually associated with patient noncompliance, diabetes, or use of nicotine like smoking and chewing tobacco.
Outcomes
Most people do very well and return to prior activities and function. By six weeks, patients are extremely comfortable. They cannot be released to full activities such as manual labor, skiing and motocross until about four months. Aggressive return to activity too early can result in re-fracture, hardware breakage or nonunion. If fractures heal unevenly, post traumatic arthritis can occur requiring a knee replacement in the future.