Anterior Lumbar Interbody Fusion (ALIF) Surgery
What is an Anterior Lumbar Interbody Fusion?
An anterior lumbar interbody fusion (ALIF) is a surgical procedure used to treat back pain that is thought to be coming from the discs. The workup for this is quite extensive and patients need to have failed conservative therapy for at least six months. The type of pain may be mechanical, meaning that it is worse when you bend forward and there may be leg pain.
Diagnosis for Patients Undergoing ALIF
In terms of diagnosing the cause of pain, an MR scan (see below where all the discs look normal except the lowest one) and a discogram is typically performed.
A discogram is an invasive study that looks for a pain generator. A pain specialist under local anesthesia places needles into 3 or 4 discs spaces. He then puts saline into each one in turn. A positive result produces pain at the same disc that is abnormal on the MR scan and this is said to be concordant. If more than 1-2 are positive that’s not good. Ideally only one or perhaps two should be painful. A normal disc should cause no pain. The type of pain produced is also important. It should be close to or exactly like the bad pain that is trying to be addressed. If it is significantly different that is not a good prognosticator.
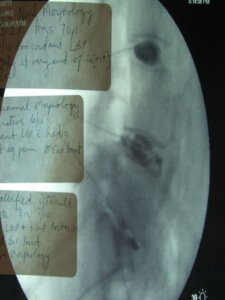
Anterior lumbar interbody fusions (ALIFs) discogram
Understanding Lumbar Anatomy
The lower back or lumbar spine is composed of five bones, called vertebrae and the sacrum. Each vertebrae is connected to each adjacent vertebrae by three joints, one at the front (anteriorly) and two at the back (posteriorly). The joint at the front is called an intervertebral disc and is a common cause of surgical pathology. The joints at the back are called facet joints and are present as pairs straddling the midline.
In addition to these three joints and bony structures, there are numerous ligaments and muscles. One of the more important ligaments is called the ligamentum flavum. This yellow ligament bridges between adjacent vertebrae and can thicken with age and cause compression of nerves. The spinal cord sits inside a bony tunnel in the posterior half of each vertebrae which is called the spinal canal. The ligamentum flavum lines the back half of this canal. The back half of the spinal canal is formed by wing shaped pieces of bone called laminae.
At each level, two lamina united and form a spinous process which is like a midline keel of bone and can be felt in the midline through the skin in the back. Holes at regular levels on each side of the spinal canal form intervertebral foramina. Each foramen allows one nerve to exit and in the lumbar spine there are five on each side. The spinal cord finishes at the lower border of the first lumbar vertebra and then becomes a leash of nerves (the cauda equina). Below this point only nerves are present, and no spinal cord is present.
Consequently, most surgery on the lower back is on and around nerves rather than spinal cord. The spinal nerves in the lumbar spine supply strength in the legs, sensation from the groin down and bladder and bowel function. Injury to one nerve may cause no problem or may affect some or all of the previously mentioned modalities.
How Does Spinal Fusion Work?
Fusion literally translates “to join” and in spine surgery this means that two vertebrae are joined together to make one. There are many reasons why one would perform a fusion (see below) but in essence the surgeons endeavors to trick the body into thinking that the two bones to be fused are a single bone that has broken and then sets up the right conditions so that in healing the bones heal as one.
Just as if you broke your arm, two bones with sticky ends would become one. In the arm’s case, a plaster cast is applied to hold things in place until the bones are healed, typically six weeks. In the lower back screws, plates, rods, cages and an external brace take the place of the plaster cast, and full fusion occurs after three months. The “sticky ends” in the case of the spine are the roughened surfaces of bone.
Typically bone graft, usually the marrow, is taken from the hip and placed between the roughened surfaces. Nowadays bone morphogenic protein can enhance fusions by stimulating bone growth. When bone healing occurs, new bone comes out of the roughened surfaces and migrates along the transplanted bone to bridge the area to be fused. Ironically, at 6-12 months all the transplanted bone or BMP has been replaced by new bone.
Understanding all of the above, it becomes clear that although there are a lot of screws and hardware involved, the operation essentially joins bone to bone and it takes a full 12 months to heal.
In all my patients they cannot smoke for one month prior and three months after the surgery as the healing rate of the bone (i.e. the success of the fusion) drops from 90% to 40-50%. Similarly, NSAIDs such as Celebrex or Mobic must not be taken for three months after surgery as they also reduce the fusion rate by 20%.
ALIF Technique
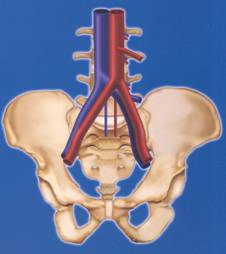
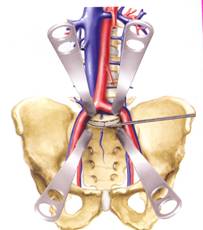
In order to perform the surgery a general surgeon is utilized to perform the anterior exposure. This is because the biggest risk from the procedure is injury to the big vessels that go to and come from the legs and the general surgeon moves the abdominal organs and vessels out of the way. The picture below shows the typical anatomy before and after an exposure.
Once the disc space is exposed the disc space is then cleaned out by the spine surgeon. surgeon. The back of the disc is not usually removed so the nerves are not seen. I then place a plastic cage into the space full of BMP and place a plate on the front. A one level case takes about an hour. Two levels take between two and three hours. Below are x-rays showing how a before and after. Note the height of the disc before and after surgery:


Use of BMP (Bone Morphogenic Protein) in Spinal Fusion Surgery
Bone morphogenic protein (BMP) is a substance commonly used when fusion surgery is done that is synthetically produced and stimulates bone growth. BMP is commonly used in all manner of fusion surgery and has reduced the incidence of fusions not taking as well as reducing the need to take bone graft from the top of the hip bone.
For years, scientists have been searching for ways to stimulate the human body to generate and repair bone more reliably and more quickly. No one appreciates the importance of such research more than the spinal surgeon. More than half of the thousands of bone fusion operations performed annually in the United States involve fusion of the spinal column. Traditionally, spinal fusion requires the transplant of bone chips from a patient’s pelvis to the spinal vertebrae to help “fuse” them together. Although this procedure can be very effective for the treatment of certain spinal disorders, the bone transplantation procedure (bone grafting) can prolong surgery, increase blood loss, increase hospital stay, increase recovery time, and increase recovery pain. Moreover, the bone grafting technique does not always reliably result in successful fusion of the vertebrae because of occasional inadequate bone growth.
Use of rhBMP-2 in Spinal Fusion Surgery
Recently, scientists and spinal surgeons have demonstrated that a genetically produced protein, recombinant human bone morphogenetic protein-2, or rhBMP-2, has the ability to stimulate a patient’s own cells to make more bone. This finding has obvious beneficial implications for the treatment of many bone fractures and bone defects. More importantly, though, rhBMP-2 can be tremendously beneficial to patients undergoing spinal fusion. It will eliminate the need for bone transplantation from the pelvis. It may more reliably and more quickly produce fusion of spinal vertebrae. It may even reduce the need for the implantation of spinal rods and screws.
The process of stimulating bone growth within the body is known as osteoinduction. One of the pioneers in the science of osteoinduction was Dr. Marshall Urist, Professor Emeritus of the Department of Orthopaedic Surgery at the UCLA school of Medicine. More than 35 years ago, Dr. Urist discovered that the proteins that directed bone to heal itself were contained within its own matrix, or substance. It was not until 1988 that these proteins were individually identified and genetically reproduced. Thereafter, it was quickly discovered that rhBMP-2 could, by itself, direct the repair and regeneration of bone in various parts of the skeleton. In several laboratory experiments performed from 1993 to 1997, rhBMP-2 was shown to effectively stimulate bone growth along spinal vertebrae.
In 1997, rhBMP-2 was used for the first time in patients undergoing spinal fusion. In this initial clinical trial, all eleven patients who had been implanted with rhBMP-2 achieved successful fusion within six months from the time of surgery. In fact, 10 of these 11 patients had achieved their fusions within 3 months of surgery. Because these patients did not require bone grafting from the pelvis, their hospital stays were shorter and their post-surgical pain was less than typically seen with the traditional bone grafting techniques. These promising initial findings are now being studied in several larger clinical trials throughout the United States.
There is little doubt that powerful biologic proteins such as rhBMP-2 will eventually help all surgical specialists treat a variety of common as well as complex spinal disorders. These osteoinductive factors will enable surgeons to modify their techniques to minimize the invasiveness of their operations. Ultimately, the goal will be reducing the pain associated with surgery and recovery, improve the effectiveness of the surgical treatments, and hasten the return of patients to productive and healthy lifestyles.
RhBMP-2 has recently received clearance from the Food and Drug Administration (FDA) for specific uses.
What are the risks and complications of Anterior Lumbar Interbody Fusion?
There are three types of risks from this surgery:
- Exposure complications: this is the commonest and most serious and this is why a general/vascular surgeon does the exposure. Anything from damage to the abdominal contents to injury to the blood vessels can occur and although uncommon can be life-threatening and require a blood transfusion
- Disc/nerve complications: Generally, the fusion rate is 95%. It drops in smokers and those with immune suppression such as kidney failure. Occasionally new neurological symptoms can develop after this surgery which may be due to stretching of nerves.
- General complications: pneumonia, clots in the legs, infections etc. can happen in all patients. These are all higher in obese patients and diabetics.
The overall complication rate is less than 5% but no guarantees can be made.
Expectations
It is difficult to look at likely success rates when the indications for surgery are quite varied. This is something that the surgeon will discuss with the patient prior to surgery. As a rule of thumb there is about a 70% chance of some improvement in back pain symptoms which can range from complete relief to not as many bad attacks.
Recovering from Anterior Lumbar Interbody Fusion
My patients spend 2-4 nights in hospital. This operation is not as sore as one done from the back, but it may take some time for the bowels to get working again. Patients are mobilized in a lumbar brace (which is basically a support for the lower back and is worn like a girdle) every time they are out of bed for a total of 3 months. At discharge all my patients do is walk. They do not bend, lift, twist or sit for prolonged periods of time. Bending and lifting are particularly bad as they can lead to screw breakage and failure of fusion. Physical therapy is not started for 12 weeks after surgery although in hospital the therapist will teach you how to get out of bed and do your daily activities. Patients are reviewed 2 weeks after surgery, then at 6 weeks, 3 months, 6 months and 1 year with x-rays. Typically, I advise my patients not to rub any creams on the incision and to keep it dry. Bathing is to be avoided, as is swimming but showering is OK. It is important that the wound is allowed to heal. Any signs of redness, discharge, swelling, etc. etc. needs to be reviewed by a doctor. Typical x-rays showing a solid fusion of the spine are shown below:

As stated in the introduction to this section, it is important not to smoke or take NSAIDs for 3 months after surgery as bone healing is occurring. Good back care is the rule for life after this surgery as, and this must be stressed, the back has not been returned to normal after a fusion.
Non-Surgical Options
An ALIF is not a small operation. Just as in lumbar discectomy there are non-operative options that include any or all of the following and these should be aggressively pursued to try and expedite improvement in symptoms:
Conservative therapy comprises of:
- Analgesia with NSAIDs (e.g. Mobic, Voltaren or Celebrex)
- Analgesia with other medications such as Tramadol
- Avoidance of bending/lifting/twisting/sitting for prolonged periods
- Physical therapy
- Hydrotherapy
- Cortisone blocks
- Possibly acupuncture
- Weight loss
- Exercise
- Bracing
Other Points
Fusing 2 bones puts stress on adjacent levels and this can accelerate wear and tear at these levels. This is important as patients can develop symptoms months or years later, which may require further surgery. The anterior approach seems to have less of this than the posterior approach as the muscles and joints of the back are not disturbed.
Why Choose Reno Orthopedic Center?
Our team of highly experienced spine doctors and surgeons are experts in treating patients suffering from back, neck and spine problems. At Reno Orthopedic Center, we use the most innovative methods and advanced procedures to deliver the best orthopedic care. Contact us to talk through your treatment options.