Spinal Injections
Dr. Lali Sekhon, MD
What are Spinal Injections?
Spinal injections comprise a less invasive, relatively conservative treatment option for back pain. They are typically considered as an option to treat back pain after a course of medications and/or physiotherapy is completed, but before surgery is considered. Injections can be useful both for providing pain relief and as a diagnostic tool to help identify the source of the patient’s back pain.
For pain relief, injections can be more effective than an oral medication because they deliver medication directly to the anatomic location that is generating the pain. Typically, a steroid medication is injected to deliver a powerful anti-inflammatory solution directly to the area that is the source of pain. Depending on the type of injection, some forms of low back pain relief may be long lasting and some may be only temporary.
Diagnostically, injections can be used to help determine which structure in the back is generating pain. If lidocaine or similar numbing medication is used, and the patient feels temporary relief after an anatomic region is injected (e.g. facet joint or sacroiliac joint), it can then be inferred that the specific region is the source of the pain. When considered in conjunction with a patient’s history, physical exam, and imaging studies, injections used for diagnostic purposes can be very helpful in guiding further treatment for the patient.
Different Kinds of Injections for Pain Relief
Common types of injections for back pain relief include:
- Epidural
- Selective nerve root block (SNRB)
- Facet joint block
- Sacroiliac Joint Injections
- Vertebroplasty
Different Kinds of Injections for Diagnosis
- Myelogram
- Discogram
Epidural Steroid Injections
Epidural steroids injections are most effective in the presence of nerve root compression. (Epidural – Space outside the dura or covering of the spinal cord. This space runs the length of the spine). The most commonly performed injection is an epidural steroid injection. In this approach, a steroid is injected directly around the dura, the sac around the nerve roots that contains cerebrospinal fluid (the fluid that the nerve roots are bathed in).
Scientific studies often demonstrate inflammation of the spinal nerves following prolonged compression, which leads to irritation and swelling. This irritation occurs at the level of the root of the lumbar nerves. The injection of steroids, which are potent anti-inflammatories, is made into the epidural space, close to the affected nerve roots. These injections must be given by experienced specialists who are well trained in this technique. Improvement of the symptoms appears to correlate well with the resolution of the nerve root inflammation. These injections are most effective when given in the first weeks of the onset of pain. Usually, two to three injections one to two weeks apart are required. Only a single injection is given if complete pain relief is achieved.
Doctors limit the number of epidural steroid injections to a maximum of three or four a year to avoid systemic side effects of the steroids. Side effects are minimal and consist mainly of mild tenderness in the area of injection which disappears in 1-2 days. Success is dependent on the cause of the pain and how long the pain has existed. The sooner the treatment is instituted, the better are the chances of getting well. This treatment, along with analgesics and physical therapy has brought relief to thousands of patients, avoiding, in the majority of cases, the need for surgery. Prior to the injection, the skin is anaesthetized by using a small needle to numb the area in the low back (a local anesthetic).
How are Epidural Steroid Injections Performed?
The patient is given a local anesthetic. The patient is placed lying on their side on the x-ray table and positioned in such a way that the doctor can best visualize the low back using x-ray guidance. The radiologist then locates, under X-ray guidance a specific spinal nerve root. A needle is introduced through the skin into the area adjacent to the nerve root. Medication is then injected into the area bathing the nerve root. The medications include an anesthetic and steroid.
What Happens After the Procedure?
Patients are then returned to a waiting room where they are monitored. Patients are then asked to record the relief they experience during the next week on a post injection evaluation sheet (“pain “diary”). This will be given to the patient when they are discharged home. A follow-up appointment will be made for a repeat block if indicated. These injections are usually done in a series of three (3), about two (2) weeks apart. The back or legs may feel weak or numb for a few hours. This is to be expected, however it does not always happen.
General Pre/Post Instructions
Patients can eat a light meal within a few hours before the procedure. If a patient is an insulin dependent diabetic, they must not change their normal eating pattern prior to the procedure. Patients may take their routine medications. (i.e. high blood pressure and diabetic medications). Patients should not take pain medications or anti-inflammatory medications the day of their procedure. A driver must accompany the patient and be responsible for getting them home. No driving is allowed the day of the procedure. Patients may return to their normal activities the day after the procedure, including returning to work.
Epidural Steroid Injection Success Rates
An epidural steroid injection is generally successful in relieving lower back pain for approximately 50% of patients. While the effects of the injection tend to be temporary (one week to one year), an epidural can be very beneficial in providing relief for patients during an episode of severe back pain and allows patients to progress in their rehabilitation.
Selective Nerve Root Block
As the spinal nerves emerge from the spinal cord, they travel laterally 1-2 cm before they exit the spine. It is at this exit (Intervertebral foramen) that these nerves are most likely compressed or “pinched” by either a herniated disc, bone spurs, narrowing of the exit secondary to calcification and decreased spacing between vertebrae (bones forming the spine). This pressure on the spinal nerves causes inflammation and pain. The pain could affect the back alone or can irradiate to the legs, which is known as sciatica.
Another common injection, a selective nerve root block (SNRB), is primarily used to diagnose the specific source of nerve root pain and, secondarily, for therapeutic relief of low back pain and/or leg pain.
When a nerve root becomes compressed and inflamed, it can produce back and/or leg pain. Occasionally, an imaging study (e.g. MRI) may not clearly show which nerve is causing the pain and an SNRB injection is performed to assist in isolating the source of pain. In addition to its diagnostic function, this type of injection for pain management can also be used as a treatment for a far lateral disc herniation (a disc that ruptures outside the spinal canal).
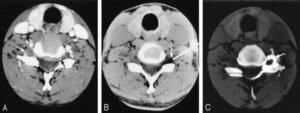
In an SNRB, the nerve is approached at the level where it exits the foramen (the hole between the vertebral bodies). The injection is done both with a steroid (an anti-inflammatory medication) and lidocaine (a numbing agent). Ct Scan is used to ensure the medication is delivered to the correct location. If the patient’s pain goes away after the injection, it can be inferred that the back pain generator is the specific nerve root that has just been injected. Following the injection, the steroid also helps reduce inflammation around the nerve root.
Success rates vary depending on the primary diagnosis and whether or not the injections are being used primarily for diagnosis. While there is no definitive research to dictate the frequency of SNRB’s, it is generally considered reasonable to limit SNRB’s to three times per year.
Technically, SNRB injections are more difficult to perform than epidural steroid injections and should be performed by experienced radiologist. Since the injection is right next to the nerve root, sometimes an SNRB will temporarily worsen the patient’s leg pain.
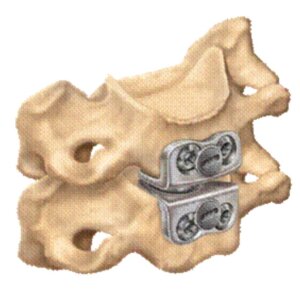
Facet Joint Injections

Facet Joints are located in the posterior spine and help to enable spinal movement. The cervical, thoracic and lumbar vertebrae each have a pair of facet joints. The facets from the upper and lower vertebrae join together (like entwined fingers) to form a facet joint. Like other joints in the body, the articulating surfaces are coated with smooth cartilage to facilitate movement. The facet joints provide stability and guide motion in the spine. If the lumbar facet joints become painful they may cause pain in the low back, abdomen, buttocks, groin or legs. If the cervical facet joints become painful they may cause pain in the head, neck, shoulders, down between the shoulder blades or in the arms.
When back pain originates from the facet joints a specific type of injection called a facet joint injection may reduce inflammation and provide pain relief. This injection involves patients with primarily low back pain (unilateral or bilateral) and no root tension signs or neurologic deficits, the pain usually being aggravated by extension of the spine. The therapeutic objective of facet joint injections is temporary relief from motion–limiting pain so the patient may proceed into an appropriate exercise program.
Doctors use fluoroscopy or CT Scans to ensure the needle is correctly placed before the medicines are injected.
The Expected Results
A facet joint injection serves several purposes. First, by placing numbing medicine into the joint, the amount of immediate pain relief experienced will help confirm or deny the joint as a source of pain. Additionally, the temporary relief of the numbing medicine may better allow a doctor or physical therapist to treat that joint. Also, time release cortisone (steroid) will help to reduce any inflammation that may exist within the joint(s).
The only test that can prove that the facet joint is the source of pain is a diagnostic facet joint block, as CT scan, X-Ray and MRI are usually unremarkable. In contrast to a treatment or therapeutic block (injection) in which a steroid is used, a diagnostic injection only uses a local anaesthetic. It is at all times preferable that the specific offending joint be identified so that a targeted therapeutic injection can be offered.
Sacroiliac Joint Injection
The sacroiliac facet joints are a small joint in the region of the low back and buttocks where the pelvis actually joins with the spine. If the joints become painful they may cause pain in the low back, buttocks, abdomen, groin or legs
Although not usually a primary pain generator, the sacroiliac joint is a common area of referred pain and can persist as the primary focus of pain. The typical pain referral pattern is to an area around and just caudal to the posterior superior iliac spine. The S-1 joint should therefore be treated within the context of the entire spine and kinetic chain, including the pelvis, hips, and lower extremities.
In patients who have failed four to six weeks of a comprehensive exercise program, local icing, mobilization/manipulation and anti-inflammatories, a sacroiliac joint injection can be helpful for both diagnostic and therapeutic purposes. In some patients, S-1 joint injections can provide significant pain relief.
When sacroiliac joint injections are employed, they should be performed with fluoroscopic guidance using contrast medium to ensure proper needle and medication placement. If helpful, they may be repeated; however, the frequency of these injections should be limited with attention placed on the comprehensive exercise program.
It should be noted that nerve blocks are not the best treatment for all pain problems. Even when they are appropriate, they are usually more effective as a part of a comprehensive treatment strategy. Such a strategy may involve medications, physical therapy, occupational therapy, stress management, relaxation training, acupuncture, or other treatments.
Vertebroplasty
Vertebroplasty is an image-guided, minimally invasive, nonsurgical therapy used to strengthen a broken vertebra (spinal bone) that has been weakened by osteoporosis or, less commonly, cancer. Vertebroplasty can increase the patient’s functional abilities, allow a return to the previous level of activity, and prevent further vertebral collapse. It is usually successful at alleviating the pain caused by a compression fracture. Performed as a day patient, vertebroplasty is accomplished by injecting an orthopaedic cement mixture through a needle into the fractured bone.
What are Some Common Uses of Vertebroplasty?
Vertebroplasty is used to treat pain caused by osteoporotic compression fractures. After menopause, women are especially vulnerable to bone loss. More than one-fourth of women over age 65 will develop a vertebral fracture due to osteoporosis. Older people suffering from compression fractures tend to become less mobile, and decreased mobility accelerates bone loss. High doses of pain medication, especially narcotic drugs, further limit functional ability. Vertebroplasty is often performed on patients too elderly or frail to tolerate open spinal surgery, or with bones too weak for surgical spinal repair. Patients with vertebral damage due to a malignant tumor may sometimes benefit from vertebroplasty. In rare cases, it can be used in younger patients whose osteoporosis is caused by long-term steroid treatment or a metabolic disorder. Typically, vertebroplasty is recommended after simpler treatments, such as bedrest, a back brace or pain medication, have been ineffective, or once medications have begun to cause other problems, such as stomach ulcers.
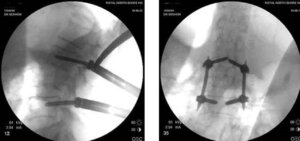
How is Vertebroplasty Performed?
Vertebroplasty is generally performed in the morning. You will be sedated and receive a local anaesthetic to numb the skin and the muscles near the spinal fracture. Intravenous antibiotics may also be administered to prevent infection. Through a small incision and guided by a fluoroscope, a hollow needle is passed through the spinal muscles until its tip is precisely positioned within the fractured vertebra. Once the needle is shown to be in the proper location, the orthopaedic cement is injected. Medical-grade cement hardens quickly, over the next 10-20 minutes. A CT scan may be performed at the end of the procedure to check the distribution of the cement. The longest part of vertebroplasty involves setting up the equipment and making sure the needle is perfectly positioned in the collapsed vertebra.
Vertebroplasty usually takes less than two hours (longer if more than one site is being treated). Although you will not be allowed to drive after the procedure, you can go home with an adult.
How Effective is Vertebroplasty?
Vertebroplasty is highly effective because after osteoporosis has made bones very porous, the cement fills the spaces and strengthens the bone so it is less likely to fracture again. After vertebroplasty, the cement stabilizes the fracture, which is thought to provide the pain relief. Patients begin regaining mobility within 24 hours and are usually able to reduce, or even eliminate, their pain medication.
For two or three days afterwards, you may feel a bit sore at the point of the needle insertion. You can use an icepack to relieve any discomfort, but be sure to protect your skin from the ice with a cloth; use the pack for only 15 minutes per hour. The tiny incision will be closed with a strip of tape, and covered with a bandage, which should remain on for several days. It’s important that the injection site remain clean. You can shower while the bandage is still on.
Bedrest is recommended for the first 24 hours following vertebroplasty, though you can get up to use the bathroom. Increase your activity gradually, and resume all your regular medications. If you take blood thinners, check with your doctor, but you may be able to restart them the day after the procedure.
What are the Benefits vs. Risks?
Benefits
Because the pain of a compression fracture is alleviated by vertebroplasty, patients feel significant relief almost immediately. After just a few weeks, two-thirds of patients are able to lower their doses of pain medication significantly. Many patients become symptom-free.
About 75% of patients regain lost mobility and become more active, which helps combat osteoporosis. After vertebroplasty, patients who had been immobile can get out of bed, reducing their risk of pneumonia. Increased activity builds more muscle strength, further encouraging mobility.
Risks
Usually, vertebroplasty is a safe and effective procedure.
- A small amount of orthopedic cement can leak out of the vertebral body. This does not usually cause a serious problem, unless the leakage moves into a potentially dangerous location such as the spinal canal.
- Other possible complications include infection, bleeding, increased back pain, and neurological symptoms such as numbness or tingling. Paralysis is extremely rare. Sometimes, the procedure causes another fracture in the spine or ribs.
What are the Limitations of Vertebroplasty?
- Vertebroplasty is not used for herniated disks or arthritic back pain.
- Vertebroplasty is not generally recommended for otherwise healthy younger patients, mostly because there is limited experience with cement in a vertebral body for longer time periods.
- The procedure cannot serve as a preventive treatment to help patients with osteoporosis avoid future fractures. It is used only to repair a known, non-healing compression fracture.
- Vertebroplasty will not correct an osteoporosis-induced curvature of the spine, but it may keep the curvature from worsening.
- It may be difficult for someone with severe emphysema or other lung disease to lie facedown for the one to two hours vertebroplasty requires. The healthcare team will try to make special accommodations for a patient with this type of condition.
- Patients with a healed vertebral fracture are not candidates for vertebroplasty.
Diagnostic Injections
Discography (Discogram)
What is the Disc?
The disc is a soft cushion like pad, which separates the vertebral bones of the spine. A disc may be painful when it bulges, herniates, tears or degenerates and may cause pain in the neck, mid back, lower back and arms, chest wall, abdomen or legs. Other structures in the spine may also cause similar pain such as the muscles, joints and nerves. Before performing discography, it has usually been determined that these other structures are not the sole source of pain in a patient (through history and physical examination, review of X-rays, CT Scans and / or diagnostic injection procedures).
What is Discography?
It is a test performed to review and assess the internal structure of the disc and determine whether it is the source of pain.
Utilizing X-ray guidance, this procedure involves the placement of needles into the discs, with an injection of contrast dye. CT and MRI, whilst providing images of the anatomy, cannot absolutely prove the source of a patient’s pain. A disc could be abnormal on CT and MRI images and not necessarily be the source of pain for the patient. Only Discography can determine if the disc(s) themselves are a source of pain.
Anatomical picture of the disc
X-ray image of a needle in the disc
How is Discography Performed?
The patient is given intravenous medication as a relaxant and pain reliever. A local anaesthetic is injected into the patient’s skin in the area that is being examined.
Needles are inserted into the disc under X-ray control (Fluoroscopy). Radiopaque dye is injected into the disc or discs whilst pain response is monitored. X-rays and C.T. Scans are then obtained.
Patient Selection
Your specialist will assess the need for discography and discuss this with you.
Experienced Operator
Discography is an operator-dependent procedure in which the specialist doing the procedure must use his/her clinical judgment to ascertain the suitability of a patient for discography and the significance of pain reproduction through discography.
These criteria are generally used to determine whether a particular disc is responsible for a patient’s pain symptoms. First, the injection of that disc must cause significant pain. Second, the quality of the pain must be concordant with the patient’ usual quality of pain. Thirdly, a control disc must have a negative injection.
Expected Results
- Recreation of painful symptoms if the disc(s) is abnormal.
- Confirmation of a diagnosis and/or determination of which disc(s) is the source of pain.
Therefore discography is done to identify the painful disc(s) and help the surgeon to plan the correct surgery or avoid surgery that may not be beneficial.
Myelography
Myelography is an X-ray examination of the spinal cord and the space surrounding it, called the subarachnoid space. The x-ray film, or myelogram, is taken after injecting a radiopaque contrast material through a needle placed in this space.
Myelography can demonstrate distortions of the spinal cord, the spinal canal within which it lies, and the spinal nerve roots connected to it.
Why a Myelogram?
It is an effective means of identifying spinal lesions caused by disease or trauma. It is relatively safe and painless examination.
Often Myelography is performed when other tests—such as computed tomography (CT) scans or magnetic resonance imaging (MRI) have not provided adequate information. For patients who cannot have an MRI exam for any reason, Myelography may be performed, followed by a CT scan.
Myelography can identify a herniated or ruptured intervertebral disc. A myelogram can accurately located the disc(s) involved, and show whether disc tissue is pressing on nerves connected to the spinal cord. This information is especially important when surgical treatment is a possibility.
- People with spinal arthritis sometimes develop sharp outgrowths of vertebral bone called bone spurs; these may press on spinal nerves and cause pain. Here again, a myelogram can indicate whether surgery might help. The exam also can identify a condition called spinal stenosis where the entire spinal canal is narrowed.
- Tumors may develop within the spinal cord or surrounding tissues. In addition, cancer from elsewhere in the body may spread to the spine. A myelogram will accurately locate a tumor mass in this region and may suggest the most effective treatment.
- Other conditions that may be shown by a myelogram are abnormalities of blood vessels that supply the spinal cord, and traumatic injuries.
How Should I Prepare for Myelogram?
Usually patients are advised to increase their fluid intake the day before a scheduled myelogram, as it is important to be well hydrated. Solid foods are avoided for three hours before the exam, but fluids may be continued. You should provide the radiologist with a list of drugs you are taking. Some drugs should be stopped one or two days before Myelography. They include certain antipsychotic medications, antidepressants, blood thinners, and drug that are used to treat diabetes. It is important that medical staff know if you have had seizures, or that you are—or might be— pregnant. If you smoke, stopping the day before the test will lessen the chance of your becoming nauseous or having headache after Myelography.
If you have had a severe allergic reaction to medication or anything else, or have a history of asthma, you will be watched especially carefully to check for a reaction when injecting the contrast material. Allergy to iodine-containing substances can be especially risky. If you have had kidney problems, tests should be done by your primary doctor prior to a referral for Myelography.
You will need to remove any jewelry near the area of your body being examined. After disrobing, you will be given a hospital gown to wear. Unless you are to spend the night in hospital, you should arrange to have a relative or friend take you home.
How is Myelography performed?
Myelography is done a hospital X-ray department. After lying face-down on the X-ray table, fluoroscopy is performed and images of the spine are projected onto the screen of a monitor. After locating the best placement for the needle, your skin will be cleaned and numbed with a local anesthetic.
Iodine-containing contrast material then is injected and the X-ray table is slowly tilted. During this time, the flow of contrast is monitored by fluoroscopy. X-rays then are taken while you are lying facedown. You will be asked to lay as still as possible while the table is tilted at different angles. The exam focuses on the area where you are feeling symptoms: the lower back area, the middle part of the back, or the neck. A foot rest and straps or supports will keep you from sliding out of position. A computed tomography (CT) scan sometimes is done immediately after Myelography while contrast material is still present in the spinal canal. This combination of imaging studies is known as CT Myelography.
What Will I Experience During Myelography?
You will feel a brief sting when local anesthetic is injected, and slight pressure as the spinal needle is inserted. Positioning the needle may cause occasional sharp pain. Although you may find the face-down position uncomfortable or have trouble breathing deeply or swallowing, the position is not usually maintained for very long.
When contrast material is injected you may feel some pressure or warmth. Headache, flushing, or nausea may follow contrast injection. Seizures are possible, but are rare.
Myelography itself usually takes 30 to 60 minutes, and a CT scan adds another 30-60 minutes to the total examination time. You will be encouraged to take fluids at this time to help eliminate contrast material from your body and prevent headache. You probably will be asked not to engage in strenuous physical activity or bend over for one or two days.