Posterior Cervical Fusion
What is a Posterior Cervical Fusion?
A posterior approach to the cervical spine is generally reserved for patients with myelopathy. Myelopathy literally means “sick spinal cord” and can be caused by many things, some of which are not reversible. Compression of the cord can cause myelopathy and is the commonest reason for surgical intervention. The approach is also gaining popularity for the management of trauma and tumor conditions but it is really in the management of myelopathy secondary to degenerative disease (so -called “wear and tear”) that a posterior decompression and fusion is most frequently utilized.
Cervical myelopathy does not typically cause pain. Myelopathy can be asymptomatic or can cause dysfunction in the upper or lower extremities. Typical symptoms include the loss of hand control, a feeling of heaviness in the hands or legs, stiffness in walking and unsteadiness in walking. In the degenerative spine, it is typically caused by pressure on the spinal cord. This can occur because wear and tear leads to bulging of the discs, facet joints become larger and intrude into the space for the spinal cord, and also, some people are borne with a narrow space for their spinal cord.
Anatomy
The spinal cord lives in a bony hole, the spinal canal. A posterior cervical laminectomy involves an incision on the back of the neck and bone is taken away over the spinal cord to its widest diameter. After that, a fusion is performed across the facet joints at these levels using local bone from the laminectomy, screws and plates or rods.
This is the extent of bone removal and decompression from a posterior approach (yellow) allowing for excellent spinal cord decompression. Note that this is greater than that achieved by an anterior approach (orange arrows) where the position of the vertebral arteries limits lateral exposure.
Reason For Posterior Cervical Fusion
The main reason this form of surgery is performed is to try and reduce the risk of deterioration in spinal cord function. At the extreme end, bad myelopathy patients are wheelchair bound. Coupled with this, even patients with little in the way of symptoms are more at risk of spinal cord injury. This is because the space for the spinal cord is reduced and an accident as trivial as a minor car accident can transiently narrow this space via ligamentous buckling, injuring the cord. Consequently, this surgery is primarily performed as a prophylactic procedure to stop deterioration in the future.
The added fusion has several benefits:
- It allows for a much wider decompression
- It prevents the spine falling into kyphosis, which is literally a reversal of the normal curve of the spine, a situation which leaves the spine more prone to injury.
Technique
The procedure is performed under a general anesthetic and is performed on a special table called an Jackson Operating Table which allows safe positioning of the patient as well x-ray to be used throughout the procedure. Typically it takes 2-4 hours.
The head is held in a special device the keep the neck still. This is shown below:

A cut is made in the back of the neck and the thick muscles in the back of the neck are stripped away but reattached again at the end of the operation. The most important part of the case is now removal of the bone and ligaments overlying the spinal cord. This is done very carefully with drills and fine bone-biting instruments.
Once the bone is removed along with the ligaments, screws are placed through plates ( or else connected via titanium rods). X-ray guidance allows for precise screw placement. The screws, rods or plates (so-called “hardware”) holds the bones still whilst the fusion occurs. The bone removed in the laminectomy is crunched up and placed in around the facet joints which have been roughened up and form the bed of the future fusion.
This operation does not typically require a blood transfusion.
Surgery Risks
The most disastrous complication that can occur from a posterior cervical decompression and fusion is injury to the spinal cord or death. This risk is approximately 1%. Every spinal operation has a risk of leakage of spinal fluid, infection, bleeding, hardware related problems etc. etc. and these would sit at approximately 5%. There are also general risks of clots in the legs or lungs, pneumonia, heart attack etc which is again at about 5%. All in all 90-95% do well from surgery with no complications, but no surgery can be done with zero complications.
Unlike anterior cervical fusions, posterior fusions have not been shown to be associated with as much adjacent segment wear and tear. It may be jus that this technique is new. Nevertheless the joints above and below the fusion are prone to wear and tear and may require further surgery in the future. This is uncommon.
Expectations
The aim of surgery is typically to stop progression of myelopathy and any gains are a bonus. Typically:
- 40% get better
- 40% stay the same
- 20% continue to deteriorate
The operation is best performed before the myelopathy has progressed too far. The patient who starts in a wheelchair will probably stay there. Most patients do note some improvement.
The main advantage of doing a posterior decompression with a fusion is that a wide laminectomy can be performed and consequently the compression is relieved via a single-stage procedure and a further anterior approach is not required.
Recovery
A collar is placed and this is worn for 6 weeks. I let my patients take the collar off for showers and meals as long as they hold their head still. There is marked muscle spasm in the first 1-2 weeks after surgery and so headaches and neck pain are common. These are usually management by the use of muscle relaxants and analgesia and in almost all cases, the neck pain resolves in a few weeks. Typically 2-5 nights are required in hospital to allow the pain to settle.
Typical x-rays are shown below:
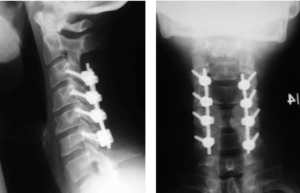
At discharge, the collar is worn for a total of six weeks. At that time flexion/extension x-rays of the cervical spine are taken and if these are satisfactory, the collar is discontinued over a period of 1-2 weeks. Initially, the neck is very stiff at this point, but with physiotherapy much of the movement returns. Because the operation is a fusion, there will always be some restriction in movement, when compared to an earlier date, but most patients do not find this restriction interferes with day to day life (see below).

(Above): This woman underwent a C3-7 fusion and decompression and is photographed six weeks after surgery, showing an excellent range of movement.
Repeat MR scanning if performed on the cervical spinal cord will show an adequate decompression of the spinal cord (see below):

BEFORE SURGERY (note compression) AFTER SURGERY (note there is space around the cord)
I will typically follow my patients for 12 months with repeat x-rays to ensure no hardware-related complications. After that time, investigations are only performed if problems occur.
Non-Surgical Options
There are very few non-surgical options in terms of the management of cervical myelopathy. The only real option is to defer surgery if the patient feels the risks outweigh the benefits. There is no guarantee that they will deteriorate if they decide not to have surgery. Because the compression of the spinal cord is structural lesion, no physiotherapy, diet or alternative therapy will relieve the compression. Chiropracty is contraindicated as spinal manipulation can lead to spinal cord injury.
Other Points
Myelopathy is common and become more so as the population ages. Cervical laminectomy with lateral mass fusion is the most recent operation available to the spinal surgeon in the management of multilevel spinal cord compression. Because the compression is from the back as well as the front, artificial disc surgery may not be adequate to deal with this pathology is some patients, and here a laminectomy and fusion may indicated.