Cervical Artificial Disc Surgery
What is a Disc?
The spine is a column that is made of up bones, discs and ligaments. The blocks of bone (or vertebrae) provide the anterior support and structure of the spine. The discs are in between the bones and act like a “shock absorber” between the vertebrae. The discs also contribute to the flexibility and mobility of the spinal column. The discs are made up of two parts:
- The inner portion of the disc is a jelly-like material and is called the nucleus pulposus and
- The outer part, called the annulus fibrosus of the disc, is stronger and more fibrous. The anulus fibrosus surrounds and supports the inner jelly material.
Disc material is mainly composed of water and other proteins. As a normal part of aging, the water content gradually reduces. This can cause the disc to flatten out and even develop tears or cracks throughout the annulus fibrosus. These discs are often referred to as “degenerative” discs and may or may not cause pain.
In the case of a degenerative disc, the inner jelly material (the nucleus pulposus) can bulge out and press up against the annulus fibrosus. This can stimulate the pain receptors causing pain to occur. The cracks or tears that develop within the annulus fibrosus can also become a source of pain. Finally, the inner nucleus can also come out through the cracks in the annulus and compress nerves or spinal cord, a condition that may cause weakness, pain, pins and needles or numbness, and may require surgery.
Current Treatment Options for Prolapsed Discs
Non-surgical options for people with disc protrusions in the neck include rest, heat, pain medications and physiotherapy. When non-surgical treatment options fail, surgery is often the next step. This usually means spinal fusion surgery. Neck pain with compression of the nerves in the neck or spinal cord is a common condition that affects the spine and may require surgery. If only nerves are compressed, with symptoms in one arm, a period of conservative management is instituted and if this fails surgery is contemplated. Early surgery is performed if there is severe weakness or pain that cannot be effectively controlled with available analgesia. If the spinal cord is being compressed, surgery to decompress the spinal cord is usually recommended. This compression can be caused by bulging disc or bony spurs.
Surgery on the spinal cord is performed either from the back of the neck (laminectomy) or through the front of the neck (cervical discectomy or vertebrectomy). If the compression of the spinal cord is from the front, then the decompression must be done from the front (anterior decompression). Typically, if the entire disc is removed, a wedge of bone is taken from the hip and put into its place, possibly with a plate and screws to hold it into place (see below). This is commonly referred to as an anterior cervical decompression and fusion.

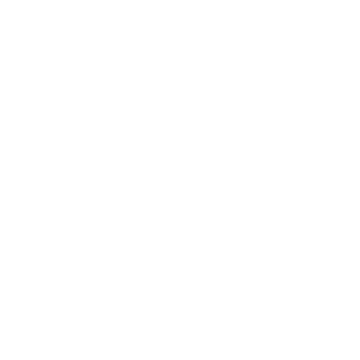
(Above left): MRI scan of the cervical spine showing a typical disc protrusion between the 5th and 6th cervical vertebra compressing the spinal cord
(Above middle): A Schematic diagram of a typical anterior discectomy and fusion procedure. A block of bone graft is placed into the space left when the disc is removed
(Above right): A postoperative x-ray on the patient shown to the left. The disc has been removed, a block of bone has fused the 5th and 6th vertebrae and a plate with screws holds it into place
This is a common operation and often no bone graft from the hip is taken nowadays. Instead, bone from a bone bank (donated cadaver bone called allograft) or plastic cages filled with bone substitutes are used. Whilst it takes pressure off the spinal cord, it necessitates that at least 2 of 7 bones in the neck are fused. This does reduce some of the movement in the neck, but patients typically do not notice it unless several levels are fused. Typically, after this surgery, the patients were a neck brace for 6 weeks.
The problem with fusing bones in the neck is that adjacent levels in the neck are placed under more strain. This has increased “wear and tear” at the surrounding disc space levels has been termed “adjacent segment stenosis”. We now know that if 10 people have a single level fusion, at 10 years 3 have had to have another operation for narrowing at the next level either above or below. Secondly, the bone does not always heal or “fuse” correctly. In fact, the overall success rates for these procedures range from 48% to 89%. Finally, spinal fusion at one or more levels increases stress to the rest of the spine. This transferred stress may cause new problems to develop at the other levels, which may lead to additional surgery.
There are clear reasons for not putting in artificial disc and doing a fusion instead.
Click here to download a brochure explaining why.
Cervical Disc Replacement Instead of Cervical Fusion
A new technique which has been available throughout the world since 2001 is removing the disc and then replacing it with an artificial disc. This has 2 main benefits:
- Motion is maintained and the patient will not feel a restriction in the range of motion.
- Theoretically adjacent segment disease will not occur.
Consequently, patients undergoing decompression and placement of an artificial cervical disc do not need a brace after surgery and may need less surgeries on their neck in the future.
The idea of spinal disc replacement is not new. It was first attempted 40 years ago when implanted stainless steel balls were implanted into the disc spaces of over 100 patients. These pioneering efforts were followed by more than a decade of research on the degenerative processes of the spine, spinal biomechanics and biomaterials before serious efforts to produce an artificial disc resumed. The Bryan cervical disc prosthesis represents a state-of-the-art disc prosthesis, although several are now available. A newer prosthesis, termed Prestige LP® (see below), is also available, outside the US) working as a ball and socket system. The choice is made by the surgeon and tailored to your spine. Worldwide there are at least a dozen in place.
Prestige Cervical Disc System

The Prestige Disc is the first artificial cervical disc that will be available in the US. The is a ball and trough design and mimics normal cervical motion. It is made of stainless steel, so postoperative MR scans have a lot of artifact. It is secured to the bone with screws and is useable for one level disease only. The FDA study comparing Prestige to fusion was favorable for the disc.
Bryan Cervical Disc System
The Bryan Cervical Disc System is a composite type artificial disc designed with a low friction, wear resistant, elastic nucleus with two anatomically shaped metal plates. A flexible membrane forms a sealed space and contains a lubricant to reduce friction and wear and tear. The implant allows for normal range of motion and comes in five sizes. Expect US release in 2008

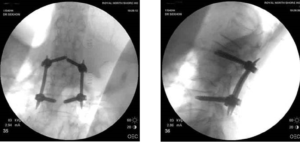
(Above) X-rays of the cervical spine after implantation of an artificial disc. Normal movement is preserved.
The initial clinical experience with the Bryan Total Cervical Disc Prosthesis has been promising.
(Above left): The Bryan artificial disc prosthesis.
(Above right): A skeletal model of the cervical spine showing how the artificial disc is placed.
When Not to Have an Artificial Disc (click here)
Key Points
- The selection of patients for this surgery is very particular and left to very specialized spinal surgeons
- We do not yet know the long-term outcomes of having an artificial disc for 50+ years
- Over 10000 artificial discs have been placed in patients in worldwide over the past 5 years
- Not all patients are suitable for artificial disc surgery
More information:
- The aim is to keep movement at the level of surgery so that extra stress is not placed at the adjacent level.
- The operation is best for arm pain (80-90% likely to improve)
- The risk of something disastrous happening from the surgery such as death or quadriplegia/cord injury is 1-2%. The risk of other complications is about 5-10% which included the risks of swallowing or voice problems, which may or may not be permanent, infection, bleeding etc. etc. These are the same risks as an ACDF but the 20% morbidity from the hip graft, if used, is avoided.
- All my patients who receive an artificial disc are informed that if, during the surgery, it is not possible to place the artificial disc, then a fusion is done. This happens in less than 5% of cases, but you must be prepared for this.
- If you underwent surgery, you would need to x-ray of your neck in flexion and extension at six weeks, three months, six months then yearly after surgery. No collar is required postoperatively, and you could return to work as soon as one week postoperatively.
- If you have a short neck, it may not be possible to place the prosthesis.
- The long-term results with artificial discs are not yet known. We do know that hip and knee replacements do wear out and the same may happen with this prosthesis- at this stage we just don’t know. It may take 10-20 years to find out. Significantly, very few have been removed to date.